Proximal Tibiofibular Ligament Instability
Diane Low OMS4, Brian Gilmer, MD
Anatomy and Biomechanics of the Proximal Tibiofibular Joint
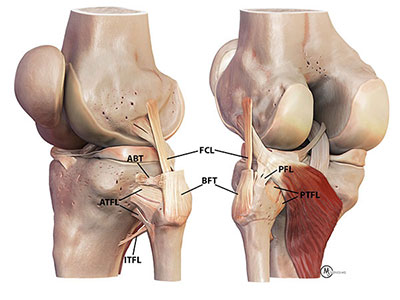
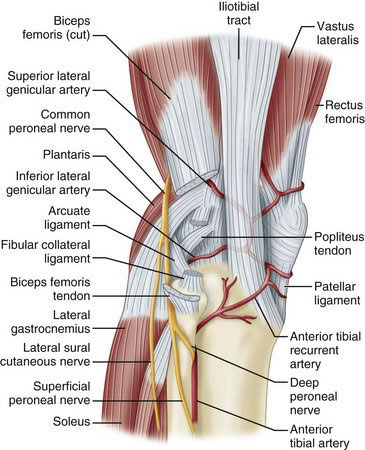
- The proximal tibiofibular joint (PTFJ) is the articulation of the lateral tibial plateau of the tibia and the head of the fibula. The fibular head lies in an angled groove behind the lateral tibial ridge, which helps to prevent anterior fibular movement with knee flexion [7]. The proximal fibula moves posteromedial with knee extension. The anterolateral and posteromedial sliding movement of this joint reduces torsional forces from the ankle, prevents lateral bending of the tibia, spreads the axial load while standing, and helps to stabilize the knee [2]. The PTFJ capsule is stabilized by anterior and posterior tibiofibular ligaments, lateral collateral ligament, popliteus, and biceps femoris tendon (BFT). The lateral collateral ligament compresses the fibular head to the tibia and is tight from 0° to 30° of knee flexion. A layer of the biceps femoris tendon wraps anteriorly to the anterior PTFL to insert onto Gerdy's tubercle, which is where the IT band attaches on the tibia. This reinforces the joint with anterolateral movement of the fibular head.
- Just below the tibiofibular ligaments is the common peroneal nerve that wraps around the fibular neck. This nerve divides into superficial and deep branches to innervate the muscles in the leg that dorsiflex and evert the foot.
- The articular surface of the PTFJ could be described as horizontal or oblique. The horizontal orientation has a greater surface area, <20° of joint inclination, and increased rotatory mobility, which decreases the rate of injury [5]. The oblique variant has an angle of inclination >20° and is often constrained especially with rotation. The angle of inclination can reach up to 76° decreasing the surface area of the joint, which predisposes to instability [7].
Proximal Tibiofibular Ligament Instability
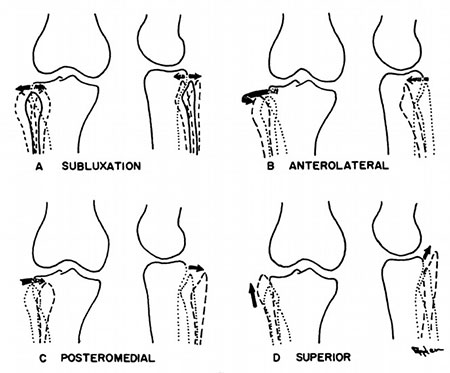
- There are acute and chronic causes of instability with four patterns: anterolateral dislocation, posteromedial dislocation, superior dislocation, and atraumatic subluxation. Anterolateral dislocation is the most common and is caused by a violent twisting of the flexed knee with the foot inverted and plantarflexed. The lateral collateral ligament and biceps femoris tendons relax when the knee is flexed to at least 30 degrees, which allows the fibula to move anteriorly. This decreases the joint’s stability. Inversion and plantarflexion of the foot pulls on the peroneal muscles, which are attached to the fibula and foot, and causes the fibula to dislocate anteriorly tearing the posterior tibiofibular ligaments.
- On the other hand, posteromedial dislocations occur after a direct blow to the proximal fibula from an anterior to posterior direction or a twisting injury. The twisting movement tears the joint capsule and stabilizing ligaments nearby. This dislocation commonly injures the common peroneal nerve causing a foot drop.
- Superior dislocations are found with high energy ankle injuries that damage the interosseous membrane between the tibia and fibula [5].
- Lastly, atraumatic subluxation is excessive anterior posterior movement of the joint. This is often seen in preadolescent girls with ligamentous hyperlaxity. There are no specific exercises for proximal tibiofibular joint instability because there are no muscles that control the joint. The bicep femoris attaches to the fibular head but is not able to hold the joint stable with deep flexion or rotational activities with the knee bent [4].
Presentation
History
- This ligamentous instability is most commonly seen in 20 to 40 year old athletes who play sports that involve violent twisting of the flexed knee. Such sports include wrestling, parachute jumping, judo, gymnastics, skiing, rugby, football, soccer, track, baseball, basketball, racquetball, and roller skating. This acute injury causes swelling to the lateral knee. Any of the four patterns of PTFJ instability can cause lateral knee pain especially with pressure on the head of the fibula. Patients are often unable to bear weight onto that leg and have pain with ankle and knee movement. Clicking or popping, no pain with daily activities, and a sensation of instability with sudden changes in direction with deep squatting can be seen in chronic dislocations of the joint.
Physical Exam
- Upon physical exam of an acute injury, lateral knee swelling will be observed. Pain around the fibular head is accentuated by dorsiflexing and everting the foot along with knee flexion. There may be pain in the popliteus and biceps femoris tendons. Check for lateral collateral ligament stability when the knee is in full extension by translating the proximal fibula anteriorly and posteriorly. Rădulescu sign will be seen when the patient is prone, the thigh and the knee flexed to 90°, the leg is rotated internally, and attempt to subluxate the fibula anterolaterally. Chronic or atraumatic injuries have tenderness and or apprehension when translating the proximal fibula in anterior and posterior directions with 90˚ of knee flexion.
Imaging
- Lateral and AP x-rays of the knee are often taken. On the lateral x-ray, the fibular head should be behind the posteromedial portion of the lateral tibial condyle known as the Resnick’s line. Displacement of the fibular head will disrupt this relationship. There are variable degrees of knee rotation on the lateral x-ray so an x-ray with 45-60 degrees of internal rotation is preferable for the PTFJ [5]. On the AP radiograph, half of the fibula head should be behind the lateral margin of the lateral tibial condyle. In an anterolateral dislocation the fibula will have less than half of its head overlapped. Axial computed tomography is the most accurate imaging to detect a proximal tibiofibular joint injury. Subtle proximal dislocations can be missed so comparison with the contralateral knee may improve detection.


Treatment
- In acute anterolateral dislocation cases, immobilization in a brace in full extension for 3 weeks allows the posterior proximal tibiofibular joint ligament tear to scar in [4]. In chronic cases, the proximal tibiofibular ligament is reconstructed with a graft. A tunnel through the fibular head and another tunnel in the tibia are drilled where the proximal posterior tibiofibular joint ligaments were. The hamstring allograft or autograft is pulled through the tunnels and screwed into the tibia and fibula [4].
- Post-op care consists of immobilization during ambulation and non-weight or toe-touch weight bearing for 6 weeks. This ensures the new ligament heals in place and will not stretch out. The knee range of motion for the first 2 weeks is from 0˚ to 90˚. After 6 weeks, crutches will no longer be needed if there is no limp with ambulation. Exercises to strengthen the quadriceps should be done. Avoid sitting cross-legged, squatting beyond 70˚ of knee flexion, and squatting with twisting for 4 months postoperatively. Most patients can return to full activities between four to six months postoperatively if there is adequate restoration of the joint’s stability, pain relief, and return of strength [4].
References
- Azar, F. M., & Miller, R. H., III. (2016, June 5). Knee Injuries. Musculoskeletal Key. musculoskeletalkey.com/knee-injuries-2/
- Feger, J. (2021, April 13). Proximal tibiofibular joint. Radiopaedia.radiopaedia.org/articles/proximal-tibiofibular-joint-1?lang=us
- Forster, B. B., Lee, J. S., Kelly, S., O'Dowd, M., Munk, P. L., Andrews, G., & Marchinkow, L. (2007). Proximal tibiofibular joint: an often-forgotten cause of lateral knee pain. AJR. American journal of roentgenology, 188(4), W359–W366. doi.org/10.2214/AJR.06.0627
- LaPrade, R., MD. (2020, January 14). Proximal Tibiofibular Joint Instability. Robert LaPrade, MD | Minnesota Knee Specialist | Twin Cities, Minneapolis-St.Paul, Edina, Eagan. drrobertlaprademd.com/proximal-tibiofibular-ligament-instability/
- Meadows, M. (2021, April 1). Proximal Tibiofibular Joint Instability. Radsource.radsource.us/prox-tibfib-joint/
- Oksum, M., & Randsborg, P. H. (2018, August 2). Treatment of Instability of the Proximal Tibiofibular Joint by Dynamic Internal Fixation With a Suture Button. ScienceDirect. sciencedirect.com/science/article/pii/S2212628718301300
- Ogden J. A. (1974). Subluxation and dislocation of the proximal tibiofibular joint. The Journal of bone and joint surgery. American volume, 56(1), 145–154.
- Sekiya, J. K., & Kuhn, J. E. (2003, March). Instability of the Proximal Tibiofibular Joint. Journal of the American Academy of Orthopaedic Surgeons. journals.lww.com/jaaos/fulltext/2003/03000/instability_of_the_proximal_tibiofibular_joint.6.aspx
- Warner, B. T., Moulton, S. G., Cram, T. R., & LaPrade, R. F. (2016). Anatomic Reconstruction of the Proximal Tibiofibular Joint. Arthroscopy techniques, 5(1), e207–e210. doi.org/10.1016/j.eats.2015.11.004





















