Posterolateral Corner (PLC) Knee Injuries
Ryan Quinn, MS4, Brian Gilmer, MD
Introduction
Posterolateral corner (PLC) knee injuries commonly result from a force directed at the anteromedial aspect of the knee with the foot planted firmly on the ground1. Patients frequently complain of pain over the posterolateral aspect of the knee, and instability with normal walking, twisting, and cutting2.
These injuries are notoriously difficult to diagnose, treat and understand due to the complex anatomy comprising the posterior lateral corner (PLC) of the knee. PLC injuries comprise approximately 16 % of ligamentous knee injuries3. Nearly 75% of PLC injuries are identified with concurrent damage to either the anterior (ACL) or posterior cruciate ligament (PCL)4. The posterior cruciate ligament is more commonly damaged than the ACL in PLC injuries, as the PCL and popliteus tendon are anatomically parallel, and thus forces that will cause a PCL injury may also lead to PLC injuries2. PLC injuries are important to diagnose, as a missed diagnosis is a common cause of cruciate ligament reconstruction failure 1. Further, the operative results of PLC injuries that are repaired in the acute phase of healing are superior to chronic reconstructions5,6.
Anatomy
Anatomic components comprising the posterolateral corner of the knee serve to provide both dynamic and static stability to the posterolateral corner—preventing hyperextension, tibial external rotation and varus angulation7.
Dynamic Stabilizers
Structures that provide dynamic stability to the posterolateral knee include the iliotibial band, long and short heads of the biceps femoris muscle, and the lateral head of the gastrocnemius muscle.
Figure 1: IT Band, Short and Long Heads of Biceps Femoris and Gastrocnemius Anatomy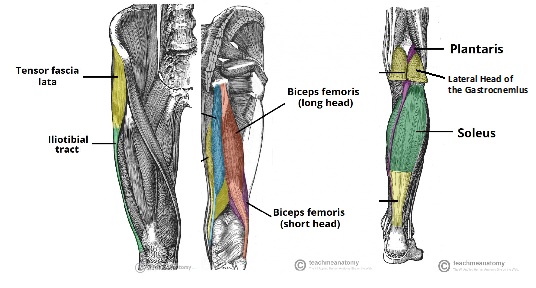 Image adapted from here
Image adapted from here
The iliotibial band originates at the anterolateral iliac tubercle portion of the external lip of the iliac crest and inserts distally at Gerdy’s tubercle on the proximal lateral tibia. It is comprised of four layers: superficial, middle, deep, and capsulo-osseus 8. Of note, an anterior expansion of the superficial layer forms the iliopatellar band, which contributes to proper patellofemoral tracking8.
The long head of biceps femoris forms the posterior aspect of tissue that covers the lateral aspect of the knee8. It has 6 attachments at the knee—2 tendinous (direct arm and anterior arm) and four fascial. The two tendinous arms are commonly avulsed from their fibular attachments in PLC injuries8. The direct tendinous arm contains the majority of the common biceps tendon insertion on the far posterolateral edge of fibular head8. The anterior tendinous arm crosses laterally over the fibular collateral ligament (FCL), forming the lateral wall of the biceps bursa-- an important surgical landmark8.
The short head of the biceps femoris originates just medial to the linea aspera of the distal femur and attaches to the anterior medial edge of the common biceps tendon. It has six insertions in total at the knee8.
The lateral gastrocnemius tendon originates on the lateral edge of the gastrocnemius muscle belly, and attaches to the fabella, posterior capsule, and to the distal femur in the region of the supracondylar process on average 13.8 mm’s posterior to the FCL insertion8,9. It is rarely damaged in PLC injuries8.
Static Stabilizers
Multiple ligaments provide static stability to the posterolateral knee—most importantly the (lateral) fibular collateral ligament, popliteus tendon, and popliteofibular ligament. Secondary static stabilizer’s include the lateral capsule ligament, the coronary ligament and the fabellofibular ligament.
Figure 2: Deep Ligament Anatomy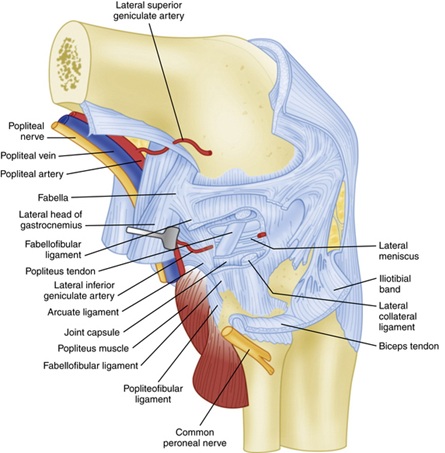 Image retrieved from here10
Image retrieved from here10
The fibular collateral ligament (FCL) originates from the femur 1.4 mm proximal and 3.1 mm posterior to the lateral epicondyle and attaches slightly anterior to the midportion of lateral aspect of the fibular head 11. The FCL is located deep to the superficial IT band and long head of biceps femoris. The FCL is the primary static stabilizer to varus opening at the knee8. Biomechanical studies have shown that there is no statistically significant increase in varus opening of the knee until the FCL is cut—even if all other ligaments have been cut8.
The popliteus muscle complex is also integral to providing static stability to the posterolateral knee. It originates on the femur at the popliteal sulcus 18.5 mm anterior to FCL attachment on average and continues distally to attach to posteromedial edge of the middle to distal posterior tibia, where the insertion is covered by the semimembranosus muscle complex8,11. It functions to internally rotate the tibia on the femur and unlock the knee during the initiation of flexion. It gives off several structures throughout its course that assist in posterolateral knee stability summarized below:
- Three popliteomeniscal fascicles (anteroinferior, posterosuperior, and posteroinferior), which form a hoop like attachment that is visible arthroscopically8. These stabilize the lateral meniscus, and thus prevent medial entrapment of lateral meniscus with varus forces to the knee8.
- A popliteofibular ligament originating at the popliteal musculotendinous junction distal to the popliteomeniscal fascicles and attaching to medial aspect of the fibular styloid8.
Figure 3: Popliteus tendon, Popliteofibular Ligament and FCL Anatomy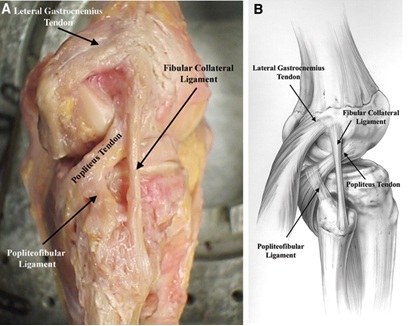 Image retrieved from here10
Image retrieved from here10
Secondary static stabilizers are listed below: The mid-third lateral capsular ligament is a thickening of the lateral capsule of the knee joint that is equivalent to the deep MCL on the medial aspect of the knee8. The fabellofibular ligament contributes static and dynamic stability at the posterolateral knee in extension and is the distal edge of the capsular arm of the short head of the biceps femoris8. Lastly, the coronary ligament is the meniscotibial portion of the posterior joint capsule that attaches the posterior horn of the lateral meniscus to the tibia8. It provides resistance to hyperextension and posterolateral rotation of the knee8.
History
Historically, the principle cause of PLC injuries has been reported to be a traumatic force to the anteromedial aspect of the knee with the foot planted on the ground, leading to a varus and hyperextension injury2,12. However, in one study by LaPrade in 1997 with 71 patients-- PLC injuries were reported with a twisting injury (30%), noncontact hyperextension (21%), contact hyperextension (15%), anterior blow to a flexed knee (10%), and a valgus blow to a flexed knee (7%)13. Thus, there is no particular mechanism of injury that will directly cause a PLC injury, and a thorough clinical exam must be performed by the physician to rule out a PLC injury in the event a knee injury.
Patients with isolated or combined PLC injuries may complain of pain over the posterolateral aspect of the knee, varus instability with normal walking, twisting, cutting, pivoting, and turning when climbing stairs, which may or may not be accompanied with swelling13. LaPrade reports from his experience that patients with isolated PLC injuries do not complain of instability going down stairs or hills, but patients with concurrent PCL tears do13.
Further, patients may complain of numbness, paresthesia’s and muscle weakness (foot drop) due to damage to the common peroneal nerve in a PLC injury2.The common peroneal nerve travels distally just deep to the iliotibial tract and biceps femoris. One study found that neurological symptoms occur in 13% of patients with PLC injuries and indicate a severe injury13.
Physical Exam
As noted above, many mechanisms can lead to a PLC injury, and a thorough physical exam is imperative in order to rule out a PLC injury—as history is not enough. In addition to inspecting the knee, palpating the knee, taking the knee through AROM and PROM, and performing a neurovascular exam-- special tests are used to diagnose PLC injuries. These include the external rotation recurvatum test, varus stress test at 30 degrees, dial test at 30 and 90 degrees, posterolateral drawer test, reverse pivot shift, and a gait exam.
In the external rotation recurvatum test, the patient lies supine and the leg is suspended by the toe. The test is positive when the lower legs falls into external rotation and knee recurvatum and varus. According to LaPrade, a positive test indicates a combined PLC and cruciate (ACL) injury14.
In the varus stress test, the patient is supine, and the knee is flexed to 30 degrees. The examiner then introduces a varus force from the ankle, with their other hand monitoring the lateral joint line for increased opening. Varus laxity at 30 degrees indicates an isolated LCL injury14. If there were to be varus laxity at 0 degrees of flexion, there is likely an LCL and cruciate injury14.
In the dial test, the patient is supine, and the knee is flexed to 30 or 90 degrees. The physician then externally rotates the ankle, creating an external rotation force at the knee. The relative external rotation of the tibial tubercle of the affected knee is qualitatively assessed in comparison to the non-affected knee. >10 degrees of external rotation at 30 degrees of knee flexion is assumed to be due to an isolated PLC injury14. If there is >10 degrees of external rotation at both 30 and 90 degrees, there is likely a PLC and cruciate injury14. This test has been criticized by some as being too subjective and is difficult to interpret14.
In the posterolateral drawer test, the patient is supine, and the hip is flexed to 45 degrees, the knee is flexed to 90 degrees and the foot is externally rotated 15 degrees14. Then, a posterolateral force is then applied to the knee, and the amount of posterolateral rotation of the tibia on the femur is qualitatively measured compared with the unaffected knee14.Anterior and posterior drawer tests should also be performed to rule out concurrent ACL and PCL injury, respectively.
In the reverse pivot shift test, the patient is supine, and the hip is flexed to 70 degrees, the knee is flexed to 70-90 degrees and the foot is externally rotated14. This leads to a posterolateral subluxation of the tibia on the femur. The knee is then slowly extended and is observed for a reduction of the tibia with a palpable clunk14.
Lastly, a gait exam should also be performed. Patients with a PLC injury will often demonstrate a varus knee thrust at the time of the foot strike in the gait cycle2,14.
Based on the above physical exam techniques, injuries are graded as minor, moderate or severe sprains based upon the Modified Hughston Criteria, summarized in the table below:
Figure 4: Modified Hughston Classification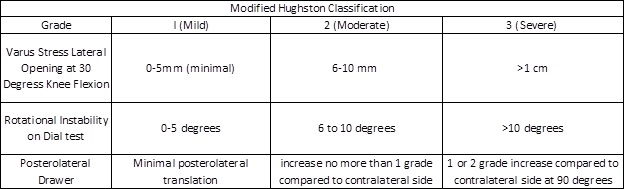
Imaging
Standard plain AP and lateral radiographs of the knee should be obtained in the setting of a suspected PLC injury14. Plain radiographs may show a Segond fracture—which is an avulsion of the meniscotibial portion of the mid third lateral capsular ligament and anterior arm of the short head of the biceps femoris off the proximal lateral tibia15, or an Arcuate fracture—which is an avulsion of the fibular styloid16.
Bilateral varus stress radiographs are also be helpful in evaluating for PLC injury. To generate this view—the patient is supine, and an angled foam block is inserted underneath the knee to obtain a standard 20 degrees of knee flexion. Then, the clinician applies a maximum varus force by placing one hand on the medial femoral condyle and one hand on the lateral aspect of the foot, and an image is taken. This is repeated on the non-injured leg, and the side to side difference (SSD) in lateral compartment gapping is calculated. Of note, it is imperative the physician provides an equal varus force to each leg to obtain an accurate result. A previous cadaveric study determined that a side to side difference > 2.7 mm to be indicative of an isolated, grade III PLC injury, and a SSD > 4 mm is indicative of a complete PLC injury17. This was considered to be the gold standard for side to side difference. However, new evidence in patients has shown that a SSD of > 2.2 mm to be indicative of a grade III FCL tear 18. The SSD is calculated as follows: the distance from the most lateral aspect of the lateral tibial plateau to the lateral tibial eminence is measured. At the midpoint of this line, a line is drawn perpendicularly towards the femoral condyle. The length of the perpendicular line is the SSD and is depicted in figure 518.
Figure 5: Varus Stress Radiographs (A: non-injured/B with combined ACL and PLC Injury18)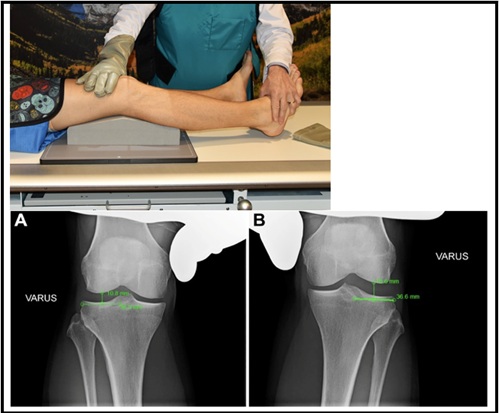
Further, in patients suspected to have a chronic PLC injury (injury > 3 weeks prior to evaluation), long leg standing radiographs are necessary to evaluate the mechanical axis of the leg for triple varus alignment (tibiofemoral bony geometry, separation of lateral compartment, and varus recurvatum)14. This view allows the physician to determine the mechanical axis and if an osteotomy is needed to support a cruciate reconstruction graft19. If the weight bearing line on this view passes within 30% of the medial side of the tibial plateau, or if triple varus alignment exists—high tibial osteotomy can be considered20.
Figure 6: Triple Varus Alignment19)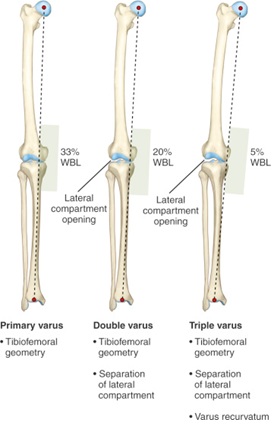
Magnetic Resonance Imaging (MRI) is also routinely ordered to evaluate soft tissue injury to the LCL, popliteus, or biceps tendon (Figure 7-Left). In the sagittal view, fluid may be recognized between the femur and popliteus, indicating that there is a PLC injury. Bone bruising may be seen in an acute setting depending on the mechanism of injury (Figure 7-Right).
Figure 7: MRI depicting PLC Injury)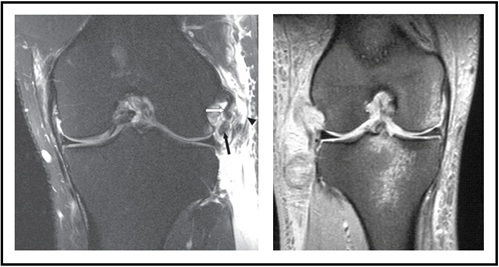 Image adapted from here
Image adapted from here
Treatment
Non-Operative Management
Non-operative management is indicated in Grade I PLC injuries, and in isolated grade II injuries5. Patient’s with Grade I or isolated II injuries recover well within three to four months the majority of the time5.
To treat the injury, the affected knee is placed in a hinged knee brace locked in extension for 3 weeks5. Weight bearing status is determined by the extent of laxity on physical exam. For mild sprains, patients may be allowed to weight bear with toe touch for the initial 3 weeks, or in more moderate injuries may be non-weight bearing for the initial 6 weeks5.
During the initial 3 weeks where the knee is immobilized in extension, quadriceps exercises, and straight leg raises should be performed daily to prevent the quadriceps muscle from shutting down21. After 3 weeks, physical therapy is started with a focus on increasing range of motion, and increasing functional activities as tolerated21. 6 weeks after the injury, patients may begin a functional rehabilitation program that includes exercise biking, leg press to max 70 degrees of knee flexion, and functional walking21. At 3 months, patients can increase activity as they are able to tolerate20.
Of note, in patients with a combined PLC and cruciate injury—the ligamentous cruciate injury should be repaired or reconstructed, and the grade I or grade II PLC injury can then be treated conservatively as above5. In this population, varus stress radiographs are indicated to assess the degree of instability of the PLC. If more laxity is noticed than expected, surgical repair or reconstruction of the PLC injury should be considered to prevent failure of the PCL or ACL graft5—as noted earlier, unrecognized PLC injuries are a potential cause of cruciate reconstruction failure.
Operative Management
Surgical intervention is indicated for both acute grade II PLC avulsion injuries, and both isolated and combined grade III PLC injuries5,21. Surgical repair or reconstruction should be completed as soon as safely possible after the injury (ideally within 2 weeks per ISAKOS [International Society of Arthroscopy, Knee Surgery and Orthopedic Sports Medicine] guidelines—Florence Italy November 2002). It has been noted that significant scar tissue can develop within 3 weeks of the injury, making identification of the superficial layer of the IT band, biceps femoris complex, and the common peroneal nerve difficult5. Performing surgery greater than 3 weeks after the injury leads to increased surgical time, tourniquet time, and a more technically challenging case5.
Operative options include a PLC repair, PLC reconstruction, or a PLC reconstruction +/- ACL reconstruction, +/- PCL reconstruction, +/- high tibial osteotomy.
PLC repair is indicated in isolated, acute grade II PLC avulsion injuries. The technique involves anatomically re-attaching the FCL, popliteus tendon, or short or long head of biceps tendon to its respective anatomical attachment site. However, repair is now generally considered an insufficient treatment, as one study noted a 37% failure rate with repair22.
PLC reconstruction, with the goal of reconstructing the FCL and popliteus tendon using a tendon graft (semitendinosus tendon) is indicated in grade III injuries, and avulsion injuries. The Mammoth Orthopaedic Institute prefers a modified LaPrade anatomic reconstruction using two grafts. The first graft reconstructs the LCL and popliteofibular ligament—attaching the graft at the femoral LCL attachment site and to the fibular head. The second graft reconstructs the popliteus tendon at the site of the femoral anatomic popliteus tendon insertion and connects the graft to the fibular head.
If a cruciate injury is present with a grade III PLC injury, PLC reconstruction should be performed at the same time as cruciate reconstruction, or prior to the cruciate reconstruction as a staged approach depending on the surgeons preference21. Further, in some patients who have triple varus alignment, a valgus high tibial osteotomy may be performed, as the bony malalignment may jeopardize the ACL or PCL reconstruction graft19,20.
Postoperative Recovery
Surgery is the start of a six to nine-month recovery process. Immediately after surgery, patients will be placed in a hinged knee brace, and placed on non-weightbearing status for 6 weeks21. During post-operative week 1 and 2, the patient is instructed to perform straight leg raises and quadriceps activation sets 4-5 times daily in the knee immobilizer brace to prevent the quadriceps from shutting down21. During this timeframe, patients should also start performing gentle range of motion exercises outside the immobilizer with goal of obtaining 90 degrees of knee flexion by the end of post op week 2 (this is surgeon dependent)21. Beginning post-operative week 3, patients are instructed to increase the repetition of quadriceps exercises and straight leg raises, to work on obtaining full knee extension multiple times daily, and also trying to increase knee range of motion past 90 degrees of flexion21. Beginning post-operative week 7, patients can begin weightbearing and closed chain strengthening exercises21. Most patients can return to activities and sports within six to nine months.
Works Cited
- LaPrade, Robert F. Posterolateral Knee Injuries Anatomy, Evaluation, and Treatment. Chapter 1: Introduction and Incidence of Posterolateral Knee Injuries. Thieme, 2006.
- LaPrade, Robert F. Posterolateral Knee Injuries Anatomy, Evaluation, and Treatment. Chapter 4: Mechanism and Presenting History of Posterolateral Knee Injuries. Thieme, 2006.
- LaPrade, R. F., Wentorf, F. A., Fritts, H., Gundry, C., & Hightower, C. D. (2007). A prospective magnetic resonance imaging study of the incidence of posterolateral and multiple ligament injuries in acute knee injuries presenting with a hemarthrosis. Arthroscopy: The Journal of Arthroscopic & Related Surgery: Official Publication of the Arthroscopy Association of North America and the International Arthroscopy Association., 23(12), 1341–1347. https://doi.org/10.1016/j.arthro.2007.07.024.
- Geeslin, A. G., & LaPrade, R. F. (2010). Location of bone bruises and other osseous injuries associated with acute grade III isolated and combined posterolateral knee injuries. The American Journal of Sports Medicine, 38(12), 2502–2508. https://doi.org/10.1177/0363546510376232.
- LaPrade, Robert F. Posterolateral Knee Injuries Anatomy, Evaluation, and Treatment. Chapter 7: treatment of Posterolateral Knee Injuries. Thieme, 2006.
- Baker, C. L., Norwood, L. A., & Hughston, J. C. (1984). Acute combined posterior cruciate and posterolateral instability of the knee. The American Journal of Sports Medicine, 12(3), 204–208. https://doi.org/10.1177/036354658401200307.
- LaPrade, R. F., Ly, T. V., Wentorf, F. A., & Engebretsen, L. (2003). The posterolateral attachments of the knee: A qualitative and quantitative morphologic analysis of the fibular collateral ligament, popliteus tendon, popliteofibular ligament, and lateral gastrocnemius tendon. The American Journal of Sports Medicine, 31(6), 854–860. https://doi.org/10.1177/03635465030310062101
- LaPrade, Robert F. Posterolateral Knee Injuries Anatomy, Evaluation, and Treatment. Chapter 3. Comprehensive Anatomy of the structures of the posterolateral knee Thieme, 2006.
- James, E. W., LaPrade, C. M., & LaPrade, R. F. (2015). Anatomy and biomechanics of the lateral side of the knee and surgical implications. Sports Medicine and Arthroscopy Review, 23(1), 2–9. https://doi.org/10.1097/JSA.0000000000000040
- Bicos, J. Purcell D, Arciero, R. Anatomic Reconstruction of the Posterolateral Corner. (2015, March 10). Clinical Gate. https://clinicalgate.com/anatomic-reconstruction-of-the-posterolateral-corner/
- LaPrade, R. F., Ly, T. V., Wentorf, F. A., & Engebretsen, L. (2003). The posterolateral attachments of the knee: A qualitative and quantitative morphologic analysis of the fibular collateral ligament, popliteus tendon, popliteofibular ligament, and lateral gastrocnemius tendon. The American Journal of Sports Medicine, 31(6), 854–860. https://doi.org/10.1177/03635465030310062101
- Hughston, J. C., Andrews, J. R., Cross, M. J., & Moschi, A. (1976). Classification of knee ligament instabilities. Part II. The lateral compartment. The Journal of Bone and Joint Surgery. American Volume, 58(2), 173–179.
- LaPrade, R. F., & Terry, G. C. (1997). Injuries to the posterolateral aspect of the knee. Association of anatomic injury patterns with clinical instability. The American Journal of Sports Medicine, 25(4), 433–438. https://doi.org/10.1177/036354659702500403
- LaPrade, Robert F. Posterolateral Knee Injuries Anatomy, Evaluation, and Treatment. Chapter 5: Clinical Examiantion of Posterolateral Knee Injuries. Thieme, 2006.
- De Maeseneer, M., Boulet, C., Willekens, I., Lenchik, L., De Mey, J., Cattrysse, E., & Shahabpour, M. (2015). Segond fracture: Involvement of the iliotibial band, anterolateral ligament, and anterior arm of the biceps femoris in knee trauma. Skeletal Radiology, 44(3), 413–421. https://doi.org/10.1007/s00256-014-2044-x
- Shindell, R., Walsh, W. M., & Connolly, J. F. (1984). Avulsion fracture of the fibula: The “arcuate sign” of posterolateral knee instability. The Nebraska Medical Journal, 69(11), 369–371.
- LaPrade, R. F., Heikes, C., Bakker, A. J., & Jakobsen, R. B. (2008). The reproducibility and repeatability of varus stress radiographs in the assessment of isolated fibular collateral ligament and grade-III posterolateral knee injuries. An in vitro biomechanical study. The Journal of Bone and Joint Surgery. American Volume, 90(10), 2069–2076. https://doi.org/10.2106/JBJS.G.00979
- Kane, P. W., Cinque, M. E., Moatshe, G., Chahla, J., DePhillipo, N. N., Provencher, M. T., & LaPrade, R. F. (2018). Fibular Collateral Ligament: Varus Stress Radiographic Analysis Using 3 Different Clinical Techniques. Orthopaedic Journal of Sports Medicine, 6(5). https://doi.org/10.1177/2325967118770170
- Noyes FR, Barber-Westin SD. Tibial and femoral osteotomy for varus and valgus knee syndromes: diagnosis, operative techniques, and clinical outcomes. In: Noyes FR, Barber-Westin SD, eds. Noyes’ Knee Disorders: Surgery, Rehabilitation, Clinical Outcomes. Philadelphia, PA: Saunders; 2017; 773–847.
- Shon, O.-J., Park, J.-W., & Kim, B.-J. (2017). Current Concepts of Posterolateral Corner Injuries of the Knee. Knee Surgery & Related Research, 29(4), 256–268. https://doi.org/10.5792/ksrr.16.029
- LaPrade, Robert F. Posterolateral Knee Injuries Anatomy, Evaluation, and Treatment. Ch. 8: Rehabilitation of Posterolateral Corner Knee Injuries and Related Surgeries. Thieme, 2006.
- Stannard, J. P., Brown, S. L., Farris, R. C., McGwin, G., & Volgas, D. A. (2005). The posterolateral corner of the knee: Repair versus reconstruction. The American Journal of Sports Medicine, 33(6), 881–888. https://doi.org/10.1177/0363546504271208





















