Maisonneuve Fracture
Jordan W. Fried, Brian Gilmer, MD, Stephen Knecht, MD
Introduction:
In 1840 Jacques Gilles Maisonneuve, a French surgeon, described the fracture pattern through cadaveric studies that is now named after him. By applying external rotation to the foot, many of the stabilizing structures of the ankle are at risk of injury.[1, 2] There is limited information available in the literature regarding this fracture pattern, but it is believed to occur more often than what is reported.[3-8] This injury is extremely important to not miss in the emergency department as it can result in poor outcomes if left untreated.[9]
Anatomy:
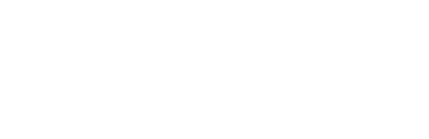
The ankle joint is composed of the distal tibia and fibula, and talus, connected by several soft tissue attachments. The ankle provides stability while adapting to the surface one walks on and allows for the ability to invert, evert, plantarflex, and dorsiflex the foot. When disrupted the patient will experience instability in their gait, with possible pain and the potential to develop early osteoarthritis. The articular surface of the ankle is formed by the joining of the superior surface of the talus, medial malleolus of the tibia, and lateral malleolus of the fibula (Figures 1a-b).
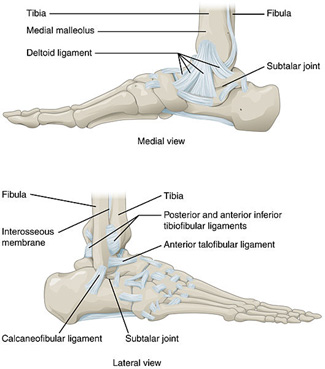 Figure 1a: Medial and Lateral Anatomic Views of the Ankle
Figure 1a: Medial and Lateral Anatomic Views of the Ankle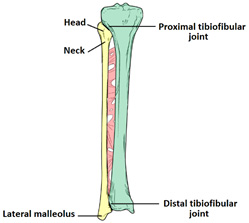 Figure 1b: Anterior Anatomic View of the Lower Leg
Figure 1b: Anterior Anatomic View of the Lower Leg
Injury:
Maisonneuve fractures are a result of external rotation of a planted foot, most often with pronation of the foot. This extreme force places significant strain on the bones and ligaments that make up the ankle joint and often results in instability. The talus externally rotates and applies stress to the medial aspect of the ankle and may cause deltoid ligament rupture or medial malleolus fracture. Acting as a wedge, the talus places pressure on the lateral malleolus and causes syndesmotic disruption between the tibia and fibula. Lastly, as the force is traveling through the deltoid ligament and medial malleolus, up towards the syndesmotic ligaments and interosseous membrane, the force generated exits the proximal fibula via fracture.
Physical Exam:
For all patients with ankle injuries, it is extremely important to rule out a Maisonneuve fracture.[9] Patients may recall a twisting motion to their ankle but not always. Patients may only report ankle pain with significant swelling, but it is important to examine the joints above and below the ankle. The “Squeeze Test” requires palpation of the tibia and fibula at the mid-calf level and if it returns positive for tenderness, it suggests a syndesmotic injury (Figure 2a). Additionally, one can perform an external rotation stress test which has the foot start in a neutral position followed by external rotation of the tibia. If there is tenderness with external rotation, syndesmotic injury is probable (Figure 2b). Proximal fibular tenderness suggests fracture. When both physical exam findings are present, Maisonneuve fracture is to be suspected.
 Figure 2a: Squeeze Test
Figure 2a: Squeeze Test Figure 2b: External Rotation Stress Test
Figure 2b: External Rotation Stress Test
Imaging:
Obtaining images at the initial visit is important to rule out a Maisonneuve fracture. Plain radiographs are vital as they can identify fibular fractures, fibular shortening, and any abnormal spacing between the tibia and fibula caused by syndesmotic disruption. Traditionally, ankle radiographs are taken in anterior-posterior (AP) view, stress view (abduction and external rotation), mortise view, and lateral view (Figures 3a-d). It is necessary to acquire AP and lateral radiographs of the knee with tibial and fibular views to determine the extent of the fibular fracture (Figures 4a-b). When reviewing the radiographs, it is important to measure the tibiofibular clear space, medial clear space, and tibiofibular overlap. The tibiofibular clear space is measured at 1 cm above the talus and measures the distance between the medial border of the fibula and the lateral border of the tibia. Typically, the tibiofibular clear space is less than 5-6 mm on the AP and mortise views. Anything greater than 10 mm is diagnostic of a syndesmotic injury.
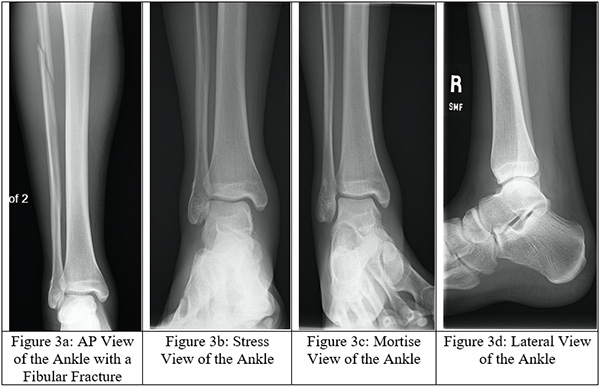
 Figure 4a: AP View of the Knee with a Fibular Fracture
Figure 4a: AP View of the Knee with a Fibular Fracture Figure 4b: Lateral View of the Knee with a Fibular Fracture
Figure 4b: Lateral View of the Knee with a Fibular Fracture
Treatment:
Non-Operative
Non-operative treatment is rarely recommended for patients with Maisonneuve fractures. Patients who qualify for non-operative intervention must either be poor surgical candidates or have no displacement of the fracture or ankle joint.[11]
Operative
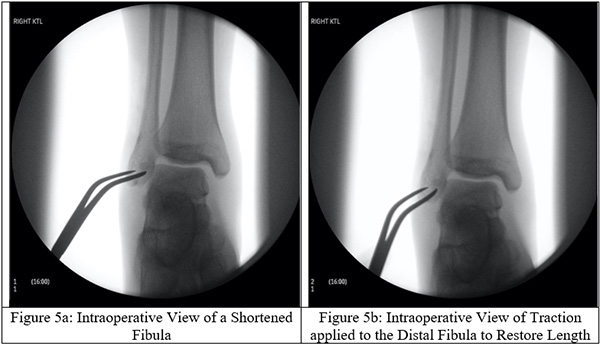
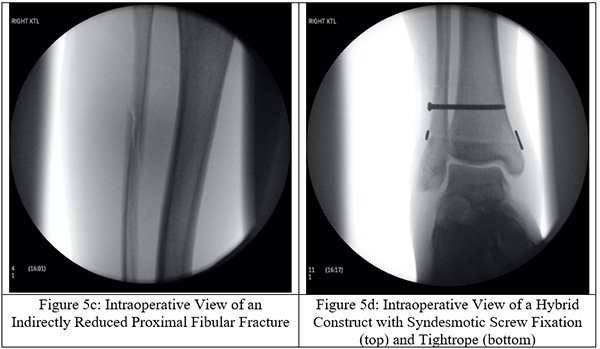
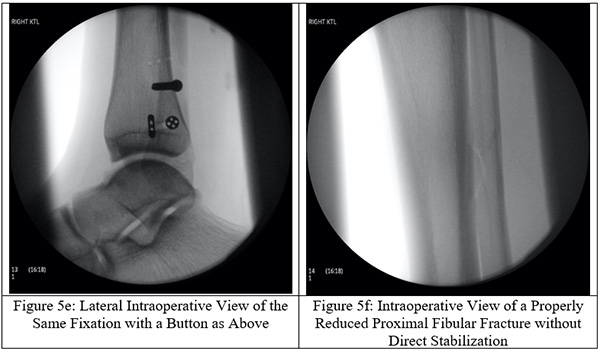
Surgical intervention is a definitive form of treatment for ankle instability and the associated fibular fracture. The proximal fibular fracture is not directly stabilized, but instead indirectly stabilized through fixating the distal fibula to the tibia with trans-syndesmotic screws (Figures 5a-f). To restore the fibular length, the distal end of the fibula is elongated into its anatomical position for trans-syndesmotic fixation. Other stabilization techniques have been described in the literature such as the use of bioabsorbable screws, syndesmotic staples, circular wire external fixators, Kirschner wires, flexible implants, syndesmotic hooks, syndesmotic bolts, and cerclage wires.[12] Metal screw fixation or a suture loop between two buttons, or some combination of the two, still stands to be the most popular choice among orthopedic surgeons. Use of screws carries the downside of requiring an additional surgery to remove the screws but may be more effective at maintaining length. By utilizing these screws, the fibular length is properly restored and the ankle mortise is appropriately reestablished. Suture loops between buttons (the ankle “tightrope”) has the advantage of not requiring screw removal but may not be as effective at maintaining fibular length.
Rehabilitation
Following surgery, patients are placed in a short removeable boot and allowed to start range of motion exercises but are not bearing weight for the first 8 weeks. Screw removal, if required is usually performed between 10-12 weeks after surgery.[1, 5, 13] A standard physical therapy program for the lower extremity can be started following screw removal.
References
- Duchesneau, S. and L.M. Fallat, The Maisonneuve fracture. J Foot Ankle Surg, 1995. 34(5): p. 422-8.
- Maisonneuve, M., Recherches sur la fracture du péroné. Arch. gén. méd., 1840. 7: p. 165-187.
- Pankovich, A.M., Maisonneuve fracture of the fibula. J Bone Joint Surg Am, 1976. 58(3): p. 337-42.
- Pankovich, A.M., Fractures of the fibula proximal to the distal tibiofibular syndesmosis. J Bone Joint Surg Am, 1978. 60(2): p. 221-9.
- Sproule, J.A., et al., Outcome after surgery for Maisonneuve fracture of the fibula. Injury, 2004. 35(8): p. 791-8.
- Inokuchi, R., et al., Maisonneuve fracture: a type of ankle fracture. BMJ Case Rep, 2019. 12(11).
- Lambers, K.T., et al., Long-term outcome of pronation-external rotation ankle fractures treated with syndesmotic screws only. J Bone Joint Surg Am, 2013. 95(17): p. e1221-7.
- Yoshimura, I., et al., Arthroscopic findings in Maisonneuve fractures. J Orthop Sci, 2008. 13(1): p. 3-6.
- Taweel, N.R., et al., The proximal fibula should be examined in all patients with ankle injury: a case series of missed maisonneuve fractures. J Emerg Med, 2013. 44(2): p. e251-5.
- Harper, M.C. and T.S. Keller, A radiographic evaluation of the tibiofibular syndesmosis. Foot Ankle, 1989. 10(3): p. 156-60.
- Stufkens, S.A., et al., Evidence-based treatment of maisonneuve fractures. J Foot Ankle Surg, 2011. 50(1): p. 62-7.
- van den Bekerom, M.P. and E.E. Raven, Current concepts review: operative techniques for stabilizing the distal tibiofibular syndesmosis. Foot Ankle Int, 2007. 28(12): p. 1302-8.
- Ebraheim, N.A., A.O. Mekhail, and S.S. Gargasz, Ankle fractures involving the fibula proximal to the distal tibiofibular syndesmosis. Foot Ankle Int, 1997. 18(8): p. 513-21.